During 2020 a number of reports highlighted a link between race and the quality of care for pregnant women. The most prominent of these came from Oxford University’s Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK unit (MBRRACE-UK) which analysed the outcomes of incidents by racial group. It found that black women were five times more likely to die in the six weeks following childbirth than white women.
Although the number of incidents was small, the difference was significant. For white women the death rate was eight in every 100,000 births, while for black women it was 40 for every 100,000 births. However, during the period studied, the rate remained consistent for white women (as well as for Chinese and Asian women) but worsened for black women and women from mixed backgrounds.
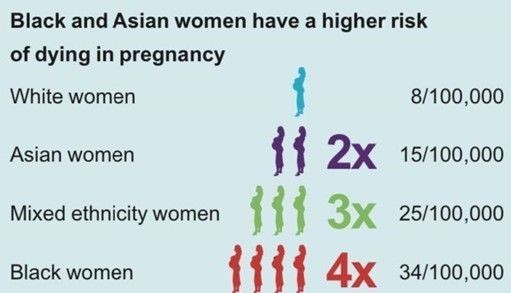
Figure 2. Disparities in maternal deaths in Black, Asian, and Mixed ethnicity women
MBBRACE-UK did not explain why this happened, since that it not their function, however they did suggest some areas that policymakers and managers should consider. These included things like:
- The socio-demographic characteristics of mothers and families
- Pre-existing physical and mental health conditions (suicide is the leading cause of maternal death in the year following birth) which may both have racial components to them.
- Inadequate utilisation of antenatal care services
- The quality of care received could have been improved
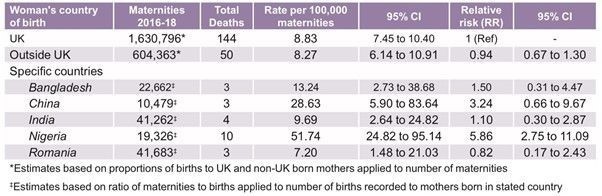
- Women born in certain countries had a significantly higher risk of death compared to those born in the UK.
According to Table 1 in the MBRRACE report the relative risk is higher for those women from India, Bangladesh, China and Nigeria.
MBRRACE-UK was not the only body to identify the problem. Public Health England also published a report on the inequality of maternity outcomes. Again, they stopped short of identifying specific causes. However, like MBRRACE-UK, they did propose some areas to consider, and the two lists had several similarities.
Public Health England’s list included issues such as:
- Socio-economic status,
- English proficiency,
- The risk of additional vulnerabilities in ethnic minorities, such as FGM or migrant
status, and cultural barriers.
- The policy of charging undocumented migrants for maternity care
- The one-size-fits-all approach of most health providers was not suitable for significant numbers of mothers and babies.
Finally, the Royal College of Obstetricians & Gynaecologists (RCOG) also pointed out the problem. In their policy position statement, also published in 2020, they noted that implicit racial bias could “negatively influence diagnosis and treatment options.” Implicit bias is unconscious and usually unintentional, but results in different racial groups receiving different treatment. One often-cited example regards pain, where clinicians often mistakenly believe that racial differences mean black people have a higher tolerance of pain, affecting pain management decisions.
Pre-existing Health Conditions Are Being Overlooked in Ethnic Minority Pregnant Women
Two serious findings of the 2020 MBRRACE report included:
- Almost 75% of women who died during or up to six weeks after pregnancy in 2016-18 had pre-existing physical or mental health conditions.
- There was little discussion regarding pre-existing mental health conditions despite the fact that 198 of those 566 i.e. 35% of women who died experienced pre-existing mental health conditions.
“Marian Knight, lead author for MBRRACE-UK and professor of maternal and child population health at the University of Oxford, said that disparity in maternal mortality simply because of a woman’s ethnicity was recognised as “unacceptable.” She added, “It is equally unacceptable for women with pre-existing medical conditions such as epilepsy to receive a lower standard of care simply because they are pregnant.”
Unfortunately, there have not been any significant moves to address the issue nationally. The Chief Medical Officer had made recommendations, for example, but the Care Quality Commission has found that most services had not implemented the recommendations, and even among those that had, the progress was reversed during the Covid-19 pandemic.
Black and ethnic minority women still face a postcode lottery when it comes to maternity, and can only hope that, lacking national action, their local maternity services are addressing the problem.
Dr Christine Ekechi, co-chair RCOG Race Equality taskforce and a consultant obstetrician and gynaecologist at Imperial Healthcare in London, U.K, commented:
“Black women are more likely to have conditions such as obesity, high blood pressure, [and] diabetes that put them at risk of having poorer outcomes in gynaecological health and subsequent outcomes.”
Maternity Negligence and Black and Ethnic Minority Women
To read the full article on the issue of black and ethnic minority women facing more negligence than white women please click here.
If mistakes were made by a nurse, midwife, GP or obstetrician or gynaecologist before or during your pregnancy or during childbirth, you could be entitled to claim compensation.
Whilst not all mistakes lead to a compensation claim, if the treatment you received fell below the standards expected from a competent medical professional and you or your baby experienced serious harm, compensation may be available.
The birth injury or negligence could be associated with:
- Inadequate monitoring of the baby or mother
- Misdiagnosing a serious condition eg. preeclampsia
- Mistakes made by a surgeon or anaesthetist eg. bladder, ureter and bowel injuries sustained during Caesarean sections.
- A poor standard of care during the delivery resulting in cuts, bruising, hip and shoulder damage and fractures to a baby
- Failure to treat or adequately treat serious post-birth complications in the mother eg. fissures, negligence associated with birth tears and /or episiotomy, poor stitching
- Failure to identify and treat secondary infections or other infections eg Group B Strep infections
- Birth injuries associated with fetal head impaction
- Placenta or parts of the placenta retained
- Mistakes made in reading CTG results on a fetal heart monitor
- Mistakes made during a breech birth or the failure to plan for a breech delivery,
Contact Devonshires Claims medical negligence solicitors for advice on making your birth injury claim.
We provide a free no-obligation case evaluation as well as a ‘No Win No Fee‘ agreement, so there are no upfront costs to start your claim and nothing to pay if your case is not successful*. To start your free case evaluation, contact our birth injury claims experts today on 0333 900 8787, email admin@devonshiresclaims.co.uk or complete our online form. Or visit: https://devonshiresclaims.co.uk/












Comments